Healthcare organizations are being squeezed from every direction: rising clinical complexity, chronic staffing pressure, expanding regulatory requirements, and patients who rightly expect safer, faster, more coordinated care. In that reality, quality management in healthcare is no longer a side initiative or an accreditation checkbox; it’s the operating system for how care is delivered every day.
Quality management in healthcare is the structured approach an organization uses to design, deliver, measure, and improve care so that it consistently meets patient needs and regulatory standards. Done well, it links strategy (clear quality aims), day-to-day operations (standard work and reliable processes), and learning (continuous improvement cycles) to reduce harm, cut variation, and lift overall performance across clinical, operational, and patient-experience domains.
This guide walks through what quality management really means in healthcare settings today, the core frameworks used globally, how to build meaningful measures, and the tools and routines required to make improvements stick rather than fade after the pilot phase. Whether you lead a hospital, manage a service line, or run a quality/innovation office, you’ll find practical ways to strengthen your quality management system and hard-wire better outcomes for patients and staff.
Table of Contents:
- What Is Quality Management in Healthcare?
- Core Frameworks Used in Healthcare Quality Management
- Measuring Healthcare Quality: What to Track
- Building a Healthcare Quality Management System (QMS): Step-by-Step
- Future of Healthcare Quality Management
- Conclusion
- Frequently Asked Questions
What Is Quality Management in Healthcare?
Quality management in healthcare is the structured approach to designing, delivering, measuring, and continuously improving care so that it consistently meets patient needs and regulatory requirements. In practical terms, it connects strategy (quality goals), operations (standard work), and learning (improvement cycles) to reduce harm, enhance patient experience, and raise clinical performance.
Unlike many industries, healthcare quality has a unique constraint: your “product” is delivered to human beings in moments of vulnerability, where errors can cause serious harm. That means quality management must integrate:
- Clinical excellence (evidence-based and effective care)
- Patient safety (reducing preventable harm)
- Patient experience (communication, responsiveness, coordination)
- Regulatory and accreditation requirements
- Equity and access (closing gaps in outcomes and experience)
Quality management also differs from one-off “quality projects.” A true quality management system establishes repeatable governance, measurement, and capability-building, ensuring continuous improvement regardless of staffing changes or leadership turnover.
Core Frameworks Used in Healthcare Quality Management
Healthcare quality management is powered by a few foundational frameworks. The best organizations don’t “pick one forever,” they combine models based on context (e.g., improvement vs. assurance vs. accreditation).
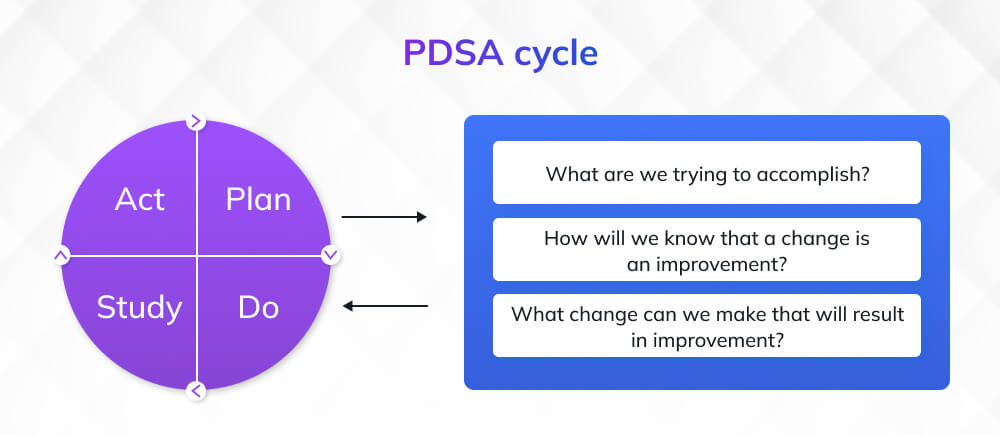
1. The Model for Improvement (IHI) and PDSA Cycles
The Model for Improvement is widely used in healthcare to accelerate improvement with a practical structure: three questions + PDSA cycles
According to IHI, the Model for Improvement includes:
- Three fundamental questions
- Plan-Do-Study-Act (PDSA) cycles to test changes and adapt them for real-world settings
It’s popular because it is lightweight, teachable, and adaptable from a single unit to an entire health system.
The three questions are:
- What are we trying to accomplish? (Aim)
- How will we know that a change is an improvement? (Measures)
- What change can we make that will improve? (Change ideas)
Then teams test changes through iterative PDSA cycles.
| PRO TIP Don’t run PDSA like a mini-waterfall project. Keep tests small (one shift, one clinician, one patient cohort), learn fast, then scale. Teams stall in “planning” and never generate learning. |
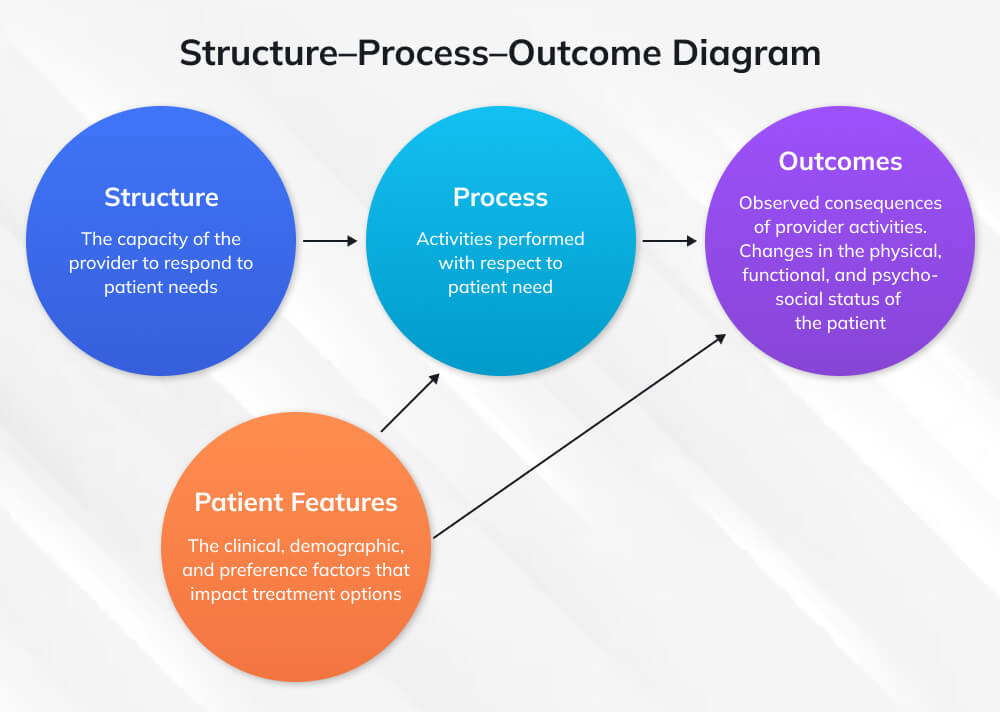
2. Measuring Quality with Structure–Process–Outcome (Donabedian)
A classic way to think about healthcare quality is the structure–process–outcome model (often attributed to Donabedian). It helps teams avoid a common trap: tracking outcomes only, without understanding the system and behaviors that drive them.
- Structure: resources and system capability (staffing, equipment, training, IT)
- Process: what clinicians and staff do (hand hygiene compliance, time-to-antibiotic)
- Outcome: results for patients (mortality, readmissions, infection rates)
3. Accreditation & Safety Goals (Joint Commission)
Many healthcare organizations anchor quality management in accreditation and safety priorities. The Joint Commission’s National Patient Safety Goals (NPSGs) were created annually to target critical patient safety areas based on input from experts and stakeholders Notably, the Joint Commission notes that effective January 1, 2026, it introduced National Performance Goals (NPGs) as a new chapter that replaces the former NPSGs. For healthcare leaders, this signals an evolution in how “beyond regulation” quality requirements are organized and measured.
| AVOID THIS MISTAKE Treating accreditation readiness as your quality strategy. Accreditation is a floor, not a ceiling. Use it to strengthen governance and reliability, but keep your improvement agenda driven by patient outcomes, equity gaps, safety risks, and experience signals. |
Measuring Healthcare Quality: What to Track
If you can’t measure quality, you can’t manage it, but measuring the wrong things can create busywork and misalignment. High-performing organizations build a balanced measurement system that includes outcomes, process reliability, experience, and (critically) learning metrics.
1. Patient Experience Measurement: HCAHPS
The HCAHPS survey is described by CMS as the first national, standardized, publicly reported survey of patients’ perspectives of hospital care CMS. CMS also explains that HCAHPS was designed to enable meaningful comparisons across hospitals and to create incentives for hospitals to improve quality through public reporting.
CMS notes that HCAHPS includes 32 questions, with 22 core questions covering domains such as nurse/doctor communication, responsiveness, discharge information, care coordination, and overall rating. This makes it a practical input into quality management, especially when teams connect low scores to specific, improvable processes (e.g., discharge education standard work).
2. Safety and Quality Indicator Systems
AHRQ provides Quality Indicators (QIs) as a way for organizations to use their own data to assist quality improvement efforts (AHRQ QIs site) AHRQ. These types of indicator sets help organizations detect opportunities for improvement, particularly around potentially avoidable complications or safety events.
How to use Indicators Well:
- Use them to spot signals, not to punish teams.
- Pair them with clinical review and operational context.
- Convert them into unit-level improvement aims (with process measures and a clear change package).
3. Building a Balanced Scorecard for Quality
A practical quality dashboard typically includes:
- Outcome Measures (patient results): mortality, complications, readmissions
- Process Measures (reliability): bundle compliance, screening completion, time-to-treatment
- Experience Measures: HCAHPS domains, complaint themes
- Equity Measures: stratify key measures by demographic variables and geography
- Operational Measures (often linked): length of stay, ED wait time, throughput
- Balancing Measures: ensure your fix doesn’t create harm elsewhere (e.g., faster discharges shouldn’t raise readmissions)
| PRO TIP When leaders ask for “one quality number,” push back. A single metric invites gaming. A balanced set (outcome + process + experience + equity + balancing) promotes honest learning. |
Building a Healthcare Quality Management System (QMS): Step-by-Step
A robust Healthcare Quality Management System (QMS) is the backbone of any successful quality improvement initiative. It ensures that improvements are not just isolated efforts but are sustainable, integrated into daily operations, and aligned with patient safety and organizational goals. Building a QMS in healthcare isn’t a one-time project; it’s a continuous, evolving system that demands a clear strategy, strong governance, and consistent data-driven decisions.
Here’s a step-by-step blueprint to help you develop a comprehensive QMS for your healthcare organization, whether you’re a hospital, clinic, or specialized care unit.
Step 1: Define Your Quality Strategy and Aims
The first step in creating a QMS is aligning your quality efforts with organizational priorities and patient needs. A well-defined quality strategy sets the stage for consistent improvements and ensures that your actions are purposeful and measurable.
- Establish Clear Aims: Identify specific, measurable, and meaningful goals that align with both patient needs and organizational capacity. These should be time-bound and realistic. For example:
- Reduce patient readmission rates by X% over the next 12 months.
- Achieve a 10% increase in patient satisfaction scores in the next quarter.
- Engage Key Stakeholders: Involve senior leadership, frontline staff, and patient representatives in goal-setting to ensure alignment across all levels of the organization.
Step 2: Establish Governance and Operating Cadence
Quality management cannot thrive without strong leadership and clear accountability. Establishing an effective governance structure is essential for driving progress and ensuring sustainability.
- Executive Sponsorship: Appoint an executive sponsor to champion quality initiatives and align them with organizational strategy.
- Quality Council Structure: Create a quality council composed of senior leaders and department heads to guide strategy, review performance, and make high-level decisions.
- Ownership Across Units: Assign specific program owners to each quality domain (e.g., safety, patient experience, clinical effectiveness) to ensure focused attention and resources.
- Operational Cadence: Set up regular performance reviews and strategy reviews (monthly and quarterly) to track progress, identify barriers, and recalibrate goals as necessary.
Step 3: Build Measurement and Data Trust
You can’t manage what you don’t measure, and in healthcare, accurate data is critical for identifying areas of improvement and tracking success.
- Define Credible Metrics: Use standardized, well-defined quality metrics, such as HCAHPS for patient experience or mortality rates for clinical effectiveness, ensuring they are relevant and actionable.
- Establish Data Trust: Ensure consistent, accurate data collection across departments and units. Data integrity and transparency are critical to making informed decisions. Trust in the system will promote engagement from all staff members.
- Build Data Pipelines: Implement reliable systems for collecting, storing, and analyzing data. Make sure the data is easily accessible to stakeholders and provides real-time insights that can inform decision-making.
Step 4: Select Change Ideas and Test with PDSA
Once you have clear goals, governance, and data systems in place, it’s time to start testing changes. The Plan-Do-Study-Act (PDSA) cycle is one of the most powerful tools for healthcare quality improvement.
- Plan: Define the problem, hypothesize potential solutions, and establish metrics for success. For example, you might aim to reduce handoff errors in the ER by implementing a standardized communication protocol.
- Do: Implement the change on a small scale. Test in one unit or shift to ensure you can learn from a manageable sample.
- Study: Collect and analyze the results to determine whether the change achieved the desired effect. If not, what needs to be adjusted?
- Act: If the change is successful, roll it out more broadly; if not, adapt your approach and re-test.
The PDSA cycle allows for rapid, iterative improvements and ensures that changes are evidence-based and scalable.
Step 5: Standardize, Train, and Sustain
When a change proves successful, it’s time to embed it into everyday practice. Standardizing improvements ensures they stick and become part of the organization’s routine.
- Convert Change into Standard Work: Once a successful change is identified, document it as standard work, such as checklists, protocols, or operating procedures, that all staff can follow.
- Train Staff: Provide ongoing training and education to staff to reinforce new practices. Incorporate them into regular orientation and continuing education programs.
- Sustainment Routines: To maintain improvements over time, set up sustainment routines, such as regular audits, feedback loops, and leadership rounding. Keep the momentum going through continuous support and reinforcement.
Step 6: Spread Improvements Responsibly
The final step in building a QMS is scaling successful changes across the organization. However, it’s important to adapt improvements to different units and departments rather than simply copying solutions.
- Adapt, Don’t Copy: What works in one unit may need adjustment to work in another. Be mindful of local context and modify processes accordingly.
- Measure and Learn: As you spread improvements, continue to measure and learn from them. Use data to track the spread’s progress and make adjustments as necessary to prevent any backslide.
Future of Healthcare Quality Management
Quality management in healthcare is shifting from “projects and reports” to true learning systems. Over the next few years, three big transitions will shape how leading organizations design and run their quality programs.
1. From Safety-Only to Whole-System Quality
Historically, “quality” often meant “patient safety plus a few indicators.” That’s no longer enough.
High-performing organizations are now treating quality as a whole-system mandate that integrates:
- Safety – preventing harm and never events
- Clinical effectiveness – delivering evidence-based care consistently
- Patient experience – communication, coordination, and respect
- Equity – closing gaps in access, outcomes, and experience
- Operational flow – ED crowding, LOS, bottlenecks that drive risk
Instead of running separate, competing initiatives (safety here, experience there, equity somewhere else), quality programs are moving toward a single, integrated agenda in which these domains are governed together and reported side by side.
2. From Static Reporting to Learning Health Systems
Most hospitals already have dashboards, scorecards, and monthly reports. The gap is not in data; it’s in what happens after the data is reviewed.
The future of healthcare quality is about turning measurement into structured learning cycles:
- Signals from HCAHPS, safety indicators, or AHRQ QIs don’t just go to a PDF—they trigger PDSA cycles, deeper review, and redesign.
- Leadership meetings shift from “explaining red dots” to asking,
- “What did we learn, what did we test, and what will we change next month?”
- Unit huddles and service-line reviews become the core engine for testing, adapting, and spreading better ways of working.
In practical terms, quality management is evolving from “compliance reporting” to continuous experimentation and adaptation, supported by real-time data rather than backward-looking summaries.
3. From “Equity as a Project” to Equity as a Core Quality Aim
Equity is moving from side initiative to a non-negotiable quality dimension.
Forward-looking organizations are:
- Stratifying key measures (readmissions, patient experience, complications, access) by race, language, gender, disability, and geography.
- Designing improvement work so that changes close gaps rather than unintentionally widen them.
- Applying frameworks like the Model for Improvement with an explicit equity lens:
- Who benefits first?
- Who might be left behind?
- How will we know if gaps are narrowing, not growing?
Regulators, payers, and boards are increasingly treating equity as part of quality, not an optional add-on. Future-ready quality programs will bake equity into aims, measures, governance, and improvement methods from day one.
Conclusion
The future of healthcare quality management is focused on transforming healthcare systems into continuous-learning environments that prioritize safety, effectiveness, patient experience, and equity, all within an integrated approach. As healthcare organizations move away from isolated safety measures and adopt a more comprehensive quality agenda, the emphasis will be on sustainable improvement rather than static reporting. The key to success lies in implementing learning systems that can adapt to real-time data, address gaps in patient experience, and promote equity across all touchpoints of the healthcare journey.
To stay ahead in this evolving landscape, healthcare professionals must stay equipped with the right skills and frameworks. Whether you are refining your quality processes, leading improvement initiatives, or spearheading patient safety measures, investing in professional development will help you navigate these changes.
To strengthen your capabilities in quality management, consider enrolling in Invensis Learning’s Lean Six Sigma Green Belt Certification. The Quality Management courses will equip you with the tools, frameworks, and knowledge to drive quality improvements, boost patient outcomes, and enhance operational efficiency in healthcare settings.
Frequently Asked Questions
1. What is quality management in healthcare?
Quality management in healthcare is the structured approach to consistently delivering safe, effective, patient-centered care by setting aims, measuring performance, improving processes, and sustaining gains. Many organizations use frameworks like the Model for Improvement with PDSA cycles to test and adapt changes.
2. What is the Model for Improvement in healthcare?
The Model for Improvement is a practical framework that uses three fundamental questions (aims, measures, change ideas) and Plan-Do-Study-Act (PDSA) cycles to accelerate improvement. It’s widely used in healthcare to test changes in real-world settings and scale what works.
3. What is HCAHPS, and why does it matter?
HCAHPS is a national, standardized, publicly reported survey of patients’ hospital care experiences. It matters because it creates comparable patient experience data, increases transparency, and creates incentives for hospitals to improve care through public reporting and value-based programs.
Q4: How do healthcare organizations measure quality effectively?
Effective measurement includes outcomes (results), process reliability, patient experience, equity stratification, and balancing measures to detect unintended consequences. Using standardized measures such as HCAHPS can strengthen comparability and credibility across hospitals.
5. What are National Patient Safety Goals?
National Patient Safety Goals are annual objectives developed by The Joint Commission to address critical patient safety areas based on input from experts and stakeholders. The Joint Commission notes that effective January 1, 2026, National Performance Goals (NPGs) replace the former NPSGs.
6. What are AHRQ Quality Indicators used for?
AHRQ Quality Indicators are measurement tools that help organizations use their data to identify potential quality and safety opportunities and support improvement work. They’re best used as signals to guide deeper analysis and local improvement projects rather than as standalone performance judgments.